Purpose:
The Symptoms-Varices-Pathophysiology (SVP) classification is a tool used for standardization and long-term assessment of Pelvic Venous Disorders (PeVD).
PeVD encompasses a group of syndromes associated with chronic pelvic pain of venous origin. These include May-Thurner syndrome, non-thrombotic iliac vein lesion (NIVL), nutcracker syndrome, pelvic congestion syndrome, and pelvic dumping syndrome. Recently, the recognition of PeVD has grown in importance. All patients with pelvic pain greater than six-months or unexplained leg symptoms should be evaluated for PeVD. Also, patients with rapid venous disease progression, neovascularization, or recurrent varicose veins after venous closure should be assessed for PeVD.
Instructions for Use:
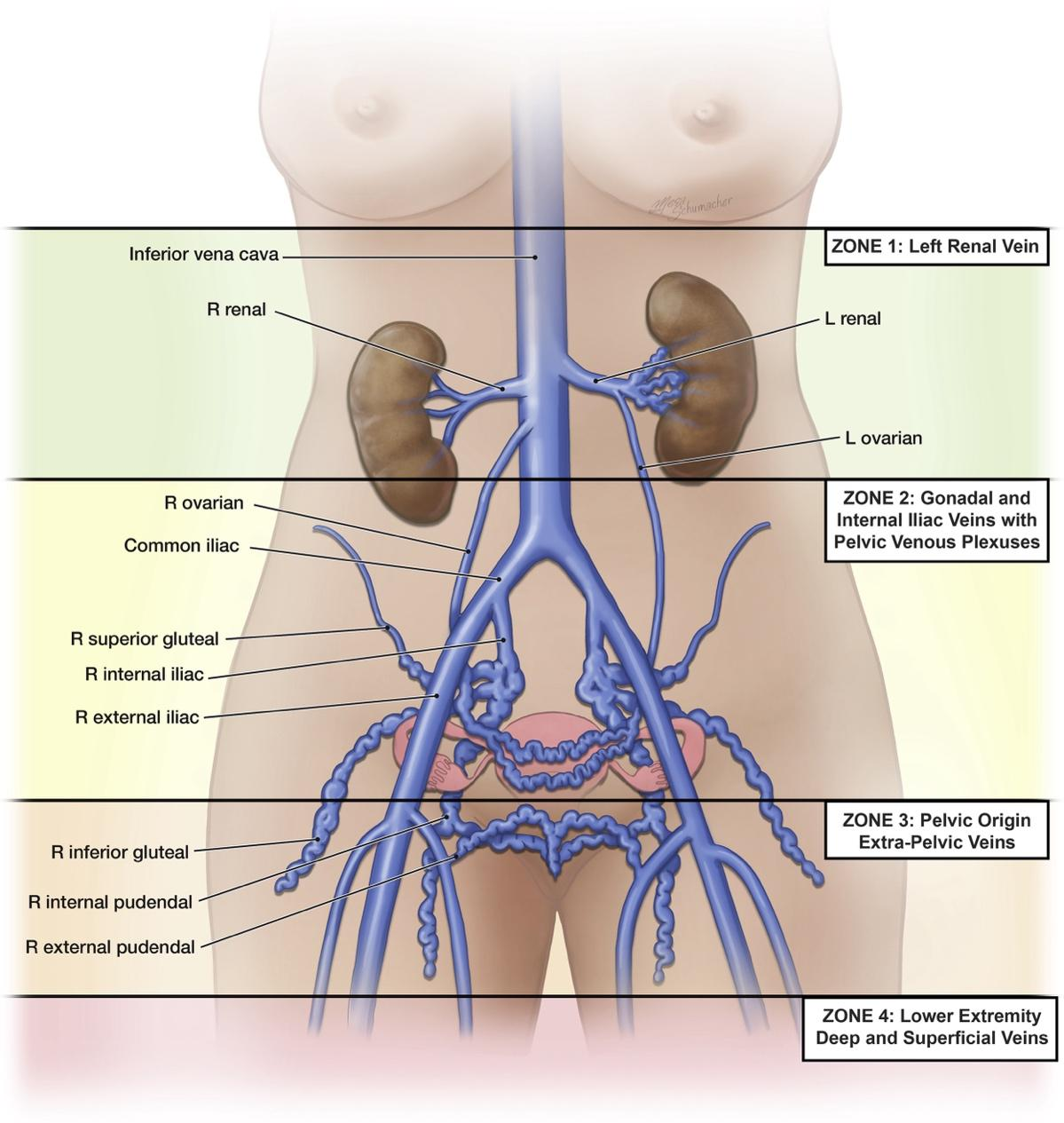
Use the SVP classification system to categorize PeVD based on the presence and severity of symptoms, extent of varices, and underlying pathophysiology. The P domain must document (A) anatomic segment, (H) hemodynamics, and (E) etiology of disease. If multiple segments are involved, each segment should be specified by a semicolon (please refer to examples). The SVP may be used at baseline and for longitudinal follow up.
Symptoms-Varices-Pathophysiology (SVP) Classification:
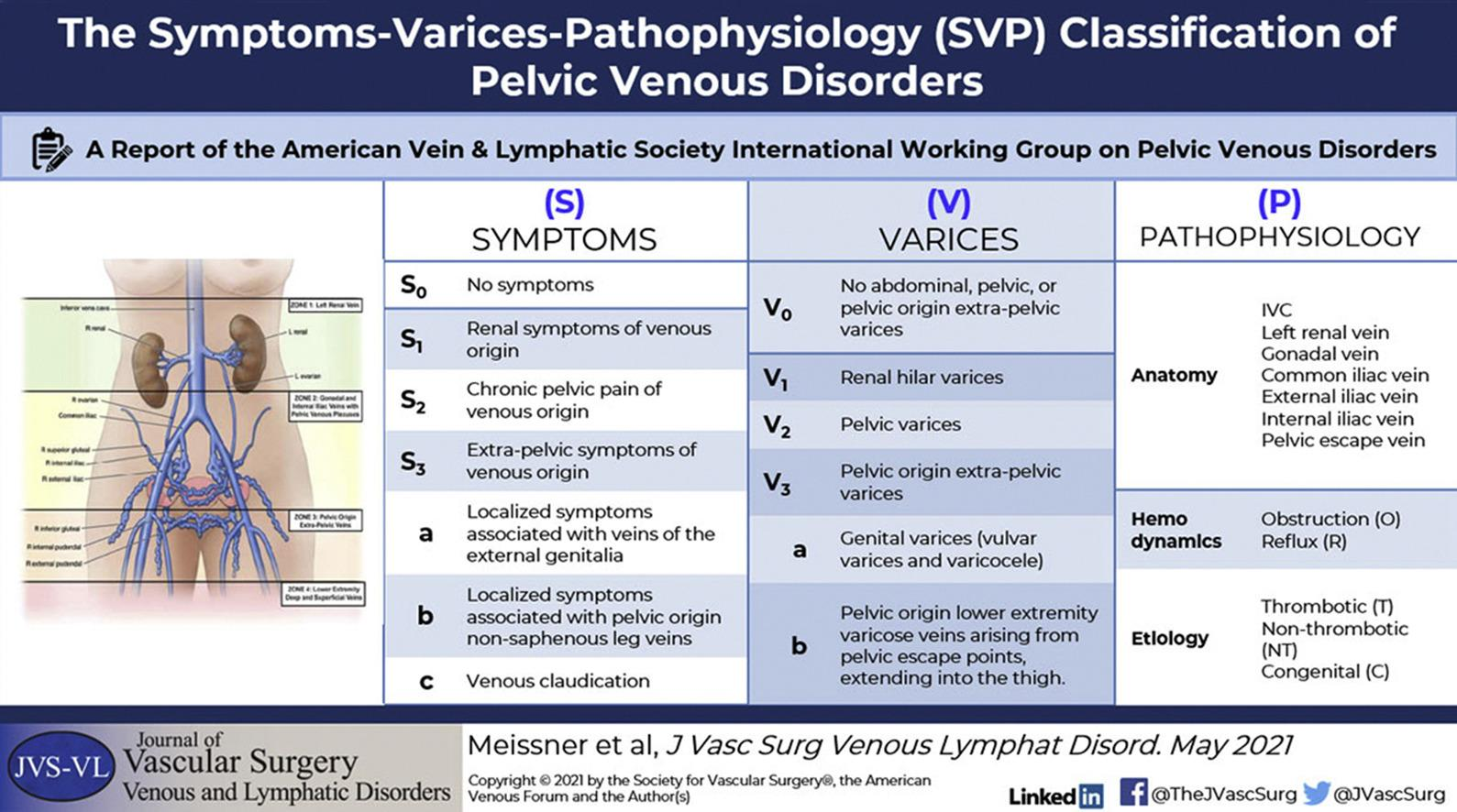
Used from Meissner et al. “The Symptoms-Varices-Pathophysiology classification of pelvic venous disorders: A report of the American Vein & Lymphatic Society International Working Group on Pelvic Venous Disorders” J Vasc Surg Venous Lymphat Disord 2021; 9: 568-584, https://doi.org/10.1016/j.jvsv.2020.12.084, with permission from Elsevier.
Examples
- Asymptomatic female presenting with NIVL of the left common iliac vein associated with internal iliac vein reflux should be designated as S0, V0, P L CIV, O, NT; L IIV, R, NT.
- Pelvic congestion syndrome with chronic pelvic pain due to bilateral ovarian vein reflux: S2, V2, P BGV, R,NT
- Nutcracker syndrome with flank pain and hematuria: S1, V1, P L RV, O, NT
- May-Thurner syndrome with left lower extremity edema: S0, V0, P L CIV, O, NT
Significance of the SVP Classification
The SVP is a standardization instrument that enhances clinical decision-making, establishes disease-specific outcome measures, and adequately categorizes patient groups for clinical trials.
References
- Meissner, M. H., et al. (2021). The Symptoms-Varices-Pathophysiology classification of pelvic venous disorders: A report of the American Vein & Lymphatic Society International Working Group on Pelvic Venous Disorders. Journal of Vascular Surgery: Venous and Lymphatic Disorders, 9(3), 568-584.
- Bałabuszek, K., Toborek, M., & Pietura, R. (2022). Comprehensive overview of the venous disorder known as pelvic congestion syndrome. Annals of Medicine, 54(1), 22-36.
- Gavrilov, S., et al. (2021). Stratification of pelvic venous reflux in patients with pelvic varicose veins. Journal of Vascular Surgery: Venous and Lymphatic Disorders, 9(5), 1417-1424.




